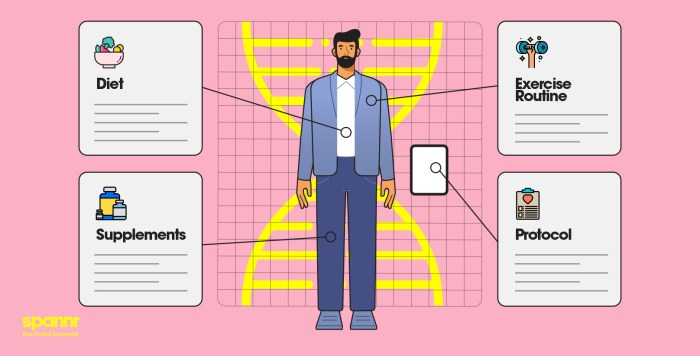
Personalized medicine is transforming the landscape of healthcare, offering tailored treatment plans that fit individual patient profiles. This innovative approach leverages genetic testing and advanced technology to customize therapies, enhancing treatment efficacy and outcomes across various health conditions.
By understanding the genetic and molecular makeup of patients, healthcare providers can devise strategies that not only target specific diseases more effectively but also minimize adverse effects. This integration of personal health data into treatment plans marks a significant shift in the way we approach medicine and patient care.
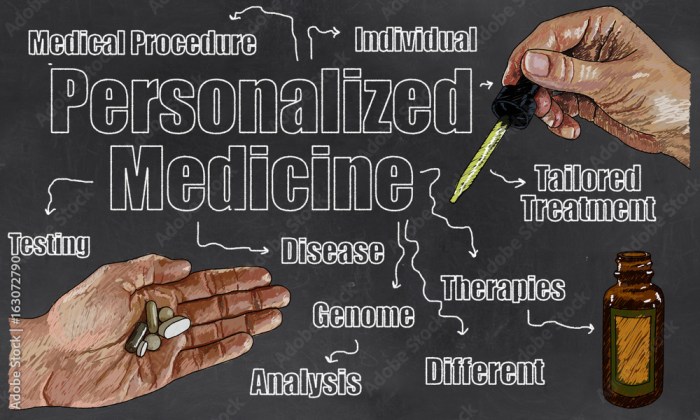
Personalized Medicine Overview
Personalized medicine, also known as precision medicine, represents a transformative approach to healthcare, where medical decisions are tailored to the individual characteristics of each patient. By focusing on genetic, environmental, and lifestyle factors, personalized medicine aims to optimize therapeutic strategies and enhance patient outcomes. This innovative paradigm is gaining traction in modern healthcare, promising a more effective and targeted treatment landscape.The foundation of personalized medicine lies in genetic testing, which plays a pivotal role in identifying specific genetic variations that influence individual responses to medications and therapies.
With advances in genomic technologies, healthcare providers can now develop more precise treatment plans based on a patient’s unique genetic makeup. This targeted approach not only improves the efficacy of treatments but also helps minimize adverse effects by ensuring that patients receive medications that are well-suited to their genetic profiles.
Role of Genetic Testing in Personalized Medicine
Genetic testing is integral to the personalized medicine framework, providing crucial insights that guide clinical decision-making. By analyzing a patient’s DNA, healthcare professionals can uncover genetic mutations and variations that may affect disease susceptibility, drug metabolism, and treatment responses. The impact of genetic testing on treatment plans is profound, as it enables the identification of potential therapeutic targets and the selection of the most suitable interventions.The significance of genetic testing is underscored by its benefits, which include:
- Enhanced treatment precision, allowing clinicians to prescribe the most effective medications based on individual genetic profiles.
- Reduced trial-and-error prescribing, leading to faster recovery times and improved patient satisfaction.
- Informed risk assessment for hereditary conditions, enabling proactive management and prevention strategies.
- Facilitation of personalized drug development, where new therapies can be tailored to specific genetic populations.
However, the implementation of personalized medicine also presents several challenges. These include:
- Cost implications, as genetic testing and personalized treatments can be significantly more expensive than standard approaches.
- Ethical concerns regarding genetic privacy and potential discrimination based on genetic information.
- Limited access to testing and treatments, particularly in underserved populations or regions.
- The need for comprehensive education and training for healthcare providers to effectively interpret genetic data and incorporate it into practice.
Incorporating genetic testing into clinical workflows necessitates a collaborative approach among healthcare professionals, patients, and genetic counselors to navigate these challenges effectively. The ongoing evolution of personalized medicine continues to reshape the landscape of healthcare, offering the potential for more effective, individualized patient care.
Personalized Medicine Applications in Various Health Areas
Personalized medicine represents a transformative approach in healthcare, tailoring treatments based on individual characteristics. This method enhances the effectiveness of therapies and minimizes adverse effects, especially in complex health conditions such as cancer and diabetes. By considering genetic, environmental, and lifestyle factors, personalized medicine enables healthcare providers to deliver more targeted and effective interventions.
Cancer Treatment
Personalized medicine is particularly impactful in oncology, where treatments can be customized based on the specific genetic makeup of a patient’s tumor. For example, targeted therapies such as trastuzumab (Herceptin) are used for breast cancer patients with HER2-positive tumors. This approach has proven to significantly improve treatment outcomes compared to traditional chemotherapy, which often affects healthy cells as well. Additionally, genomic profiling of tumors allows for the identification of specific mutations, guiding oncologists in choosing the right targeted therapy.
Recent advancements, such as CAR T-cell therapy, exemplify how personalized medicine can harness the body’s immune system to fight cancer more effectively, leading to durable responses in certain types of leukemia and lymphomas.
Diabetes Management
In diabetes care, personalized medicine enhances management strategies through the identification of genetic factors that influence insulin sensitivity and glucose metabolism. For instance, pharmacogenomics can help determine the most effective medications for individual patients, adjusting dosages to minimize side effects and optimize blood sugar control. Continuous glucose monitoring systems combined with personalized insulin regimens allow for real-time adjustments based on individual lifestyle factors, leading to improved glycemic control.
This level of customization is crucial for preventing complications associated with diabetes, such as cardiovascular disease and neuropathy.
Mental Health Treatment Strategies
Personalized medicine has begun to reshape mental health care by integrating genetic insights into treatment plans. Genetic testing can predict how individuals will respond to certain antidepressants, allowing clinicians to select medications with a higher likelihood of effectiveness. For example, variations in the CYP2D6 gene can influence the metabolism of drugs like fluoxetine (Prozac), impacting both efficacy and the risk of side effects.Moreover, therapies are increasingly tailored to the patient’s unique psychological profile, incorporating lifestyle, social, and environmental factors.
This holistic approach not only enhances therapeutic outcomes but also fosters a deeper understanding of the individual’s mental health journey.
Comparison of Pharmacology Approaches
The shift from traditional medicine to personalized pharmacology marks a significant evolution in treatment strategies. Traditional medicine often relies on a one-size-fits-all approach, prescribing standard treatments based on population averages. In contrast, personalized pharmacology employs detailed patient data, leading to a more tailored therapeutic regimen.
| Aspect | Traditional Medicine | Personalized Medicine |
|---|---|---|
| Basis of Treatment | Standardized protocols | Individual genetic and phenotypic information |
| Drug Selection | Generalized drug classes | Targeted therapies based on genetic profiling |
| Side Effect Management | Broad side effect profiles | Minimized side effects through tailored approaches |
| Outcome Predictability | Population-based outcomes | Individualized success rates |
In summary, the integration of personalized medicine across various health areas not only refines treatment protocols but also enhances patient engagement and satisfaction. This innovative approach signifies a promising shift towards more effective and individualized healthcare solutions.
Future of Personalized Medicine
The future of personalized medicine is poised to transform healthcare on multiple fronts, driven largely by technological advancements and the increasing recognition of ethical considerations. As we move forward, it’s essential to understand how innovations such as artificial intelligence (AI) and machine learning are revolutionizing the field, while also addressing important ethical dilemmas related to data privacy and accessibility. A well-thought-out roadmap will be crucial for integrating personalized medicine into mainstream healthcare systems effectively.
Technological Advancements in Personalized Medicine
The integration of AI and machine learning is at the forefront of personalized medicine, allowing for more tailored treatment options based on individual patient profiles. By analyzing vast amounts of data, these technologies can identify patterns and correlations that might be missed by human analysis alone. Some pivotal advancements include:
- Genomic Sequencing: The cost of sequencing a human genome has dramatically decreased, making it accessible for routine clinical use. This allows for personalized treatment plans based on genetic makeup.
- AI Algorithms: AI-driven algorithms can predict patient responses to various treatments, optimizing selection processes for medications or therapies.
- Wearable Technology: Devices that monitor vital signs and biochemical markers enable continuous health tracking, providing real-time data that can inform personalized treatment decisions.
- Telemedicine: Virtual consultations facilitated by AI enhance patient access to personalized care, particularly for those in remote areas.
The convergence of these technologies signifies a shift from a one-size-fits-all approach to a more nuanced understanding of individual health needs.
Ethical Considerations in Personalized Medicine
As personalized medicine evolves, ethical considerations regarding data privacy and accessibility become increasingly critical. The vast amount of data collected raises concerns about how this information is used, shared, and protected.Key ethical issues include:
- Data Privacy: Safeguarding patient information is paramount. Healthcare providers must implement robust security measures to prevent data breaches and unauthorized access.
- Informed Consent: Patients must be fully informed about how their data will be used, ensuring transparency and trust in the healthcare system.
- Equitable Access: There is a risk that personalized medicine could widen health disparities. Ensuring equitable access to advancements for all populations is essential.
- Bias in Algorithms: AI systems can inadvertently perpetuate biases if the training data is not diverse, leading to unequal treatment outcomes.
Addressing these ethical challenges is crucial for fostering public trust and ensuring that personalized medicine benefits all segments of society.
Roadmap for Integrating Personalized Medicine into Mainstream Healthcare
To effectively integrate personalized medicine into mainstream healthcare systems, a strategic roadmap focusing on education and policy changes is needed. This roadmap should Artikel actionable steps to bridge the gap between innovation and practice.Key components of the roadmap include:
- Education and Training: Medical professionals should receive training in genomics and data analytics to effectively implement personalized treatment plans.
- Policy Development: Creating regulations that govern data use and protect patient rights is vital for maintaining ethical standards.
- Public Awareness Campaigns: Informing the public about the benefits and risks associated with personalized medicine can enhance patient engagement and acceptance.
- Collaboration among Stakeholders: Partnerships between technology developers, healthcare providers, and policymakers can foster innovation and streamline the integration process.
By focusing on these areas, the healthcare system can successfully navigate the complexities of personalized medicine, ultimately leading to improved patient outcomes and enhanced healthcare delivery.
Wrap-Up
In summary, personalized medicine stands at the forefront of modern healthcare, bridging the gap between technology and individualized treatment. As we continue to explore its potential, it is crucial to address the ethical implications and work towards a framework that ensures equitable access and data security, paving the way for a healthier future for all.
Essential Questionnaire
What is personalized medicine?
Personalized medicine tailors medical treatment to the individual characteristics of each patient, often based on genetic information.
How does genetic testing contribute to personalized medicine?
Genetic testing helps identify specific genes and mutations that can influence a patient’s response to certain treatments, allowing for more effective and customized healthcare solutions.
What are the main benefits of personalized medicine?
Benefits include improved treatment efficacy, reduced side effects, and the ability to predict patient responses to therapies.
What challenges does personalized medicine face?
Challenges include high costs, limited access to genetic testing, and ethical concerns regarding data privacy and discrimination.
Will personalized medicine replace traditional medicine?
While personalized medicine will enhance traditional practices, it is expected to complement rather than completely replace them.